Retinopathy of Prematurity
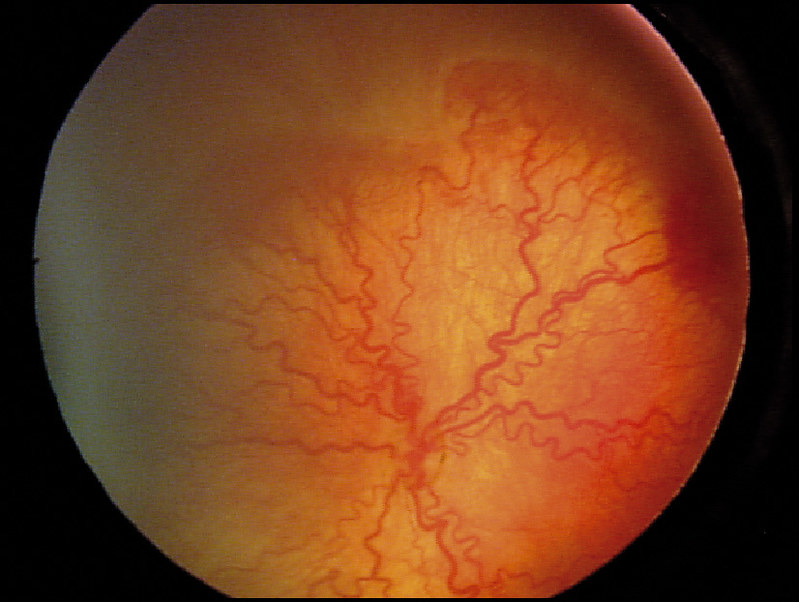
Retinopathy of Prematurity (ROP) is a disease that affects the retina (the disc at the back of the eye which processes light). Disruptions to the retina can cause problems with vision and even blindness.
ROP is when the retina doesn’t develop properly, particularly in premature babies. Abnormal growth of the blood vessels in the retina at this stage leads to vision problems. Typically this is due to the overuse of oxygen, which premature babies receive to help lung development. If oxyen is administered in an unmonitored way, it can lead to problems with the retina and ROP developing.
Around the world each year there are 15 million preterm births and over 32,000 babies became blind from ROP in 2010. Blindness in children impacts psychomotor and cognitive development, educational attainment, has negative social and financial consequences and increases the likelihood of death in childhood, in particular in low income countries (LICs).
Many intensive care units in LICs lack the resources necessary to reduce ROP. In order to prevent outcomes from the condition, premature babies should be screened by ophthalmologists weekly, who can then decide on treatment. The time window to intervene is tight, as ROP can develop and progress a few weeks after birth.
In high income countries, control strategies are effective and few infants become blind from ROP. Middle income countries in South America and Asia have shown that ROP programmes can reduce the incidence of ROP. ROP blindness is now rapidly emerging in many other LICs, including Africa, as more services that include oxygen for premature babies expand.
Key challenges in controlling ROP blindness in LICs include the low number of ophthalmologists, the extensive training required to become competent in screening and treatment, the time-consuming nature of examinations, high medico-legal risks involved and follow up of babies who have been discharged from the hospital. Services for ROP are being developed in some countries, e.g. Nigeria and Kenya, but coverage remains low due mainly to the lack of trained ophthalmologists to conduct the screening.
Telemedicine, using technology to remotely assess cases, is a potential solution as an alternative to standard screening. A trained technician or nurse at a clinic can take an image, which is then assessed by an ophthalmologist remotely at another location. This approach, which can work with low numbers of ophthalmologists, has been shown to be effective in India and Chile, but has not yet been widely implemented elsewhere.
